Mastering your digital healthcare toolkit: How to integrate solutions for a better operation
How to integrate solutions for a better operation
From routine checkups to emergencies, the healthcare sector is designed to aid those in need. But what happens when the industry itself needs help?
For years, providers and hospitals have experienced growing pressure to do more with less, straining frontline workers, support staff, and resources. Now, burnout in healthcare staff is becoming its own kind of epidemic. A 2021 survey by Kaiser Family Foundation found that 55 percent of healthcare workers who worked on the frontlines during the COVID-19 pandemic feel burned out and 49 percent feel anxious.
The industry is also dealing with an unprecedented labor shortage. Around 20 percent of healthcare workers left their positions in the past two years, including 30 percent of nurses. In the first few months of 2022, 1.7 million workers quit their healthcare jobs.
Studies predict the need for healthcare services will continue to outpace the labor market too. More than 900,000 registered nurses are expected to permanently leave their jobs between 2021 and 2026, leaving 29 states understaffed and creating major gaps between supply and demand.
Overburdened facilities offer lower quality care while the impacts of staff burnout and healthcare labor shortages ripple into every aspect of public health. These challenges are all the more difficult to address because of their consequences: poor patient experiences, increased demands on clinical staff, and higher risk of mistakes and miscommunications. With so much at stake, all eyes are on healthcare administrators to course-correct. So where can they look for help?
Digital transformation is the key to keeping healthcare organizations efficient and resilient. Though they may already use digital tools to manage patient records and staffing, many organizations need to connect their tools through an overarching platform for complete, end-to-end digitization of data and administrative workflows. These comprehensive technology solutions can make the most of staff and resources by enabling collaboration, communication, and automation — enhancing patient care and worker retention.
Over the next few chapters, we’ll provide an in-depth look at how technology for healthcare can improve operational workflows, help you automate tasks, and consolidate information; how to evaluate different solutions; and finally, how to build a complete end-to-end toolkit.
Why invest in technology for healthcare
The healthcare technology of the future is here, and new solutions enter the market to make management and care simpler all the time. With so many options to consider, healthcare organizations need a well-planned digitization strategy to ensure they make the best purchasing decisions. Simply reacting to new offerings or trends could overcomplicate processes, further straining workers and IT resources. Haphazard investment could even prevent your organization from reaping the full benefits of new technology.
That’s why you need to know exactly what your organization stands to gain from building a technology toolkit. A digital transformation strategy needs to focus on specific goals that measure the effects on patients, providers, and employees as well as the ways optimized processes impact the bottom line.
Here are some of the most important benefits of investing in technology for healthcare.

Higher productivity
Higher patient volume and rising costs over the past few decades have necessitated greater productivity. For healthcare organizations, that means more pressure to manage more patients each day without sacrificing quality of care. One of the most effective ways to achieve this ideal is by improving workflow and administrative efficiency with technology.
Medical practices that have enabled electronic health records report a range benefits, including
Survey stakeholders to identify technology gaps and opportunities
- Better overall practice management through integrated scheduling systems that link appointments to progress notes, coding, and claims
- Enhanced efficiency from centralized chart management
- Improved communication between clinicians, labs, and health plans due to
- Online access to patient data
- The ability to track electronic messages
- Digital ordering of diagnostic images and tests and digital display of results
- The ability to link to public health systems, registries, and databases
Reduced clinician burden
Switching between interacting with patients, updating documentation, and other workflow demands is incredibly taxing to providers. Adding growing patient volume and the need for faster turnaround times to healthcare providers’ regular workloads is a recipe for burnout.
Technology for healthcare providers can automate much of the busywork of record keeping so clinicians can maintain focus on patient care. On the administrative end, revamping staff scheduling processes allows providers to optimize their downtime and stay resilient. The National Library of Medicine reports that as much as 16 percent of doctors’ time is spent on tedious administrative tasks that could easily be automated, showing how paramount digital transformation is to managing healthcare burnout.
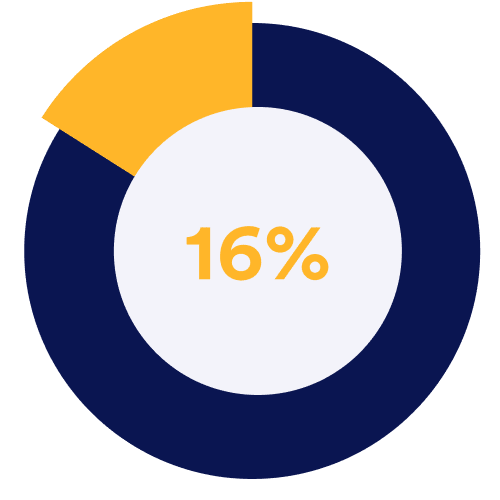
16% of doctors’ time is spent on tedious administrative tasks that could easily be automated.
Source: National Library of Medicine
Controlled administrative costs
The U.S. healthcare system spends an average of $2,500 on administrative costs per patient each year, which amounts to more than 34 percent of total healthcare spending in America.
Administrative expenses include accounting, scheduling, claims processing, and other behind-the-scenes activities that ensure smooth operations — many of which can be automated to reduce costs. In fact, McKinsey suggests that implementing digital health solutions could cut current healthcare administrative costs by 10 to 15 percent.
The U.S. healthcare system spends an average of $2,500 on administrative costs per patient each year.
Source: Annals
Better patient experience
New technology for healthcare indirectly boosts the overall patient experience — even when it’s just implemented in administrative offices. Digital check-in tools save an average of 15 minutes per appointment, getting the patient in and out more quickly for a smoother visit. When paired with telehealth technology, patients can save an average of 100 minutes of their day.
Advanced administrative technology for healthcare is needed for providers to offer the telehealth experiences patients want. According to the Centers for Disease Control (CDC), telehealth doctor visits went up by 154 % during the last week of March 2020 compared to the same week in 2019. A 2021 survey by the Memorial Sloan Kettering Cancer Center about technology and the patient experience found that 45 percent of patients now prefer telehealth appointments to in-person doctor visits. Only 34 percent prioritize an in-person visit.
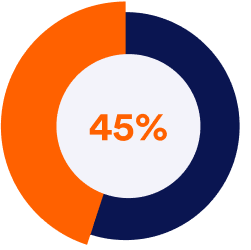
45% of patients now prefer telehealth appointments to in-person doctor visits.
Source: Journal of the National Comprehensive Cancer Network
Greater care outcomes
In 2021, McKinsey researchers reviewed over 500 studies about technology for healthcare and found that 80 percent of the papers showed an improvement in patient outcomes when digital health technology was used, especially in the management of chronic diseases. Providers understand the impact that both clinical and administrative technology for healthcare has on patients as well. Additional research by McKinsey also found that 61 percent of healthcare workers view improved patient well-being as the main driver for using digital health solutions.

What you need in a healthcare technology toolkit
New technology for healthcare can digitize every aspect of healthcare operations to streamline workflows and increase efficiency. To maximize results, organizations need to think in terms of end-to-end functionality, even though many healthcare technologies are sold as standalone software as a service (SaaS) solutions.
An effective healthcare technology toolkit consists of solutions that all work together for more seamless and automated workflows. Some solutions will primarily help administrative staff, while others will make the patient experience better, streamline communication, or just facilitate overall data management. The biggest challenge is piecing these together into one cohesive ecosystem. Dividing solutions into different categories based on their capabilities will ensure your toolkit has no gaps.
To maximize results, organizations need to think in terms of end-to-end functionality, even though many healthcare technologies are sold as standalone software as a service (SaaS) solutions support.
Here’s an overview of each of these categories and some of the capabilities you need solutions to have.
Administrative tools
Administrative technology for healthcare streamlines day-to-day operations of hospitals, clinics, and other types of healthcare organizations. Solutions should offer the following:
- Electronic health records (EHR) systems. EHR systems digitize patient files for easy management. Providers can easily access and update charts, as well as share data with other providers without using paper or physical storage space. The challenge is choosing (or building) the right one for their toolkit.
- Practice management. As the name suggests, practice management software serves as a central dashboard for day-to-day healthcare facility operations. The platform can integrate with EHR systems, third-party scheduling tools, and patient registration systems, or offer all of these capabilities itself.
- Billing. Specialty software designed for the needs of healthcare administrators will help users with both insurance billing and patient invoicing. Users can streamline workflows even further by choosing billing solutions that integrate with EHR systems, to eliminate any discrepancies between treatment and billing.
- Medical equipment planning. This specialty software automates the processes of furnishing medical offices, selecting capital equipment and calculating the total cost of ownership, and procuring medical supplies. Users can easily map out spaces, such as patient examination rooms, to ensure that selected products will fit. Many platforms also integrate with third-party product catalogs to streamline ordering.
- Marketing management. This class of software encompasses a wide array of tools, including email marketing platforms for contact list management and newsletter design, blogging and publishing tools for digital content, and social media management platforms for drafting and scheduling posts.
- Workflow/project management. Productivity and task management software has become a mainstay for every type of modern office, and many platforms are designed specifically for the needs of healthcare providers. These tools are critical for daily tasks that aren’t trackable in practice management software, including special projects.
- Security, compliance, and data privacy. Data encryption tools are vital to protecting customer and patient information in the digital economy. Technology for healthcare should always be designed with HIPAA solutions in mind. However, if you’d like to use software that isn’t built for the healthcare industry, you need specialized tools for data encryption, access permission management, and other data security details. Avoid this unnecessary complexity by choosing only software with features that support HIPAA-compliant behaviors.
Analytics tools
One of the best features of new technology for healthcare is better data collection from processes and patients. Analytics tools empower healthcare organizations to make the best use of all the information they capture. Some analytics tools to consider for your technology toolkit are these:
- Population health management. Population health tools bolster patient outcomes and provider-patient relationships. They integrate with EHR systems and analyze patient records to identify actionable insights. Based on patient data collected over time, these tools can help spot risk factors for heart disease, diabetes, and other illnesses, and then alert doctors to develop an appropriate care plan.
- Customer data management (CDM) and customer relationship management (CRM). Patient-centric database software tracks patient behavior to find opportunities to increase engagement. These platforms are often used in conjunction with marketing efforts. For example, if a hospital plans to participate in a clinical trial, administrators can use CRM to identify potential patients and reach out for recruitment.
Communications tools
New technology for healthcare is critical to communication between providers and patients as well as between administrators and staff. Your technology toolkit needs communication platforms for these audiences:
- Patient communication. These platforms encompass both apps and encrypted SMS notification systems. Apps allow providers to message patients, provide care instructions, and respond to inquiries. Facilitating this kind of personalized communication can strengthen patient adherence to medication and recovery routines, as well as retention rates. SMS platforms allow administrative staff to automatically send appointment reminders and other notifications to patients.
- Team communication. These solutions create more seamless workflows between administrators and care teams and assist these teams in coordinating care more efficiently. This can be as simple as an internal messaging platform or a more robust offering that integrates workflow management to turn messages into action items.
- Telehealth services. Video-conferencing enables HIPAA-compliant, online consults between providers and patients. After becoming more popular in the past few years, they are now a mainstay at many organizations because of the convenience they provide for patients.
Clinical tools
Technology for healthcare helps define patientprovider interactions. Consider these clinical solutions for your healthcare technology toolkit:
- Ordering and fulfillment software. These platforms automate the processes involved in prescribing medication, ordering lab tests, and gathering results. These solutions can be standalone or can integrate with EHR systems.
- Interoperability tools. Health information portability is critical to maintaining continuity of care and avoiding miscommunications or information blindspots. Providers need to be able to access or share patient information with stakeholders, within and outside the organization. Interoperability tools are any systems, apps, or other digital platforms that allow providers to facilitate this information sharing.
- Patient-generated health data apps. Often designed as smartphone apps or online portals, these platforms allow patients to record symptoms, medication adherence, and other critical information to aid providers in diagnosis and treatment. Providers can use these tools during both an initial appointment intake process or in ongoing treatment or management of a chronic illness.
- Referral and transfer-of-care portals. Some organizations still use paper forms when referring their patients to other providers. Referral portals digitize the process and make it easier to transfer care without any paper.
What to look for in technology for healthcare
Every technology category outlined in the previous section has dozens of solutions to choose from. Here are the key traits to look for as you evaluate the options:
HIPAA compliance features
HIPAA breaches are one of the biggest risks facing healthcare administrators. Over 4,419 breaches have been reported since 2009, with the annual total steadily climbing. In 2021, there were 714 breaches, compared to just 18 in 2009. Each new technology solution creates a liability issue if it doesn’t store and transmit data according to law. Look for solutions with robust security features that will enable you to meet HIPAA data protection and storage requirements. Investing in additional data security tools to engineer your own HIPAA-compliant technology suite comes at a much greater cost and effort than off-the-shelf solutions.
HIPAA breaches are one of the biggest risks facing healthcare administrators. Over 4,419 breaches have been reported since 2009.
Source: HIPAA Journal
Data Security
Online technology’s convenience and efficiency comes with additional security risks as any information that’s digitized and transmitted online becomes vulnerable to hackers. Even when organizations are fully HIPAA-compliant in their practices and technology, they are still liable for security breaches of personal health information.
In 2022, Oklahoma State University’s Center for Health Services was ordered to pay $875,000 in restitution to the U.S. Department of Health and Human Services for HIPAA violations caused by hackers. OSU staffers discovered in November 2017 that an unauthorized third party had uploaded malware into the university’s servers to access files containing patient names, Medicaid numbers, and treatment information. Further investigation revealed the third party had been accessing these files as far back as September 2016.
In 2022, Oklahoma State University’s Center for Health Services was ordered to pay $875,000 in restitution to the U.S. Department of Health and Human Services for HIPAA violations caused by hackers.
Cases like these prove that it is not enough for healthcare technology to follow HIPAA protocols — it needs to include the latest security measures to block malicious access to protected information. For example, single sign-on (SSO) protocols like Multi SSO, which allows authentication through multiple identity providers simultaneously, helps close many of the vulnerabilities that are often targeted by hackers. Additionally, following SOC 2 guidelines strengthens HIPAA-compliant solutions, providing an extra layer of security.
Ease of use
Implementing any new technology always involves overcoming the hurdle of worker adoption. Challenging already-burdened healthcare workers with learning how to use new software, apps, and other technology can create additional stress, so solutions should be as intuitive and easy to use as possible.
Solutions that require a high degree of customization through extensive coding eat up valuable IT resources, and may be difficult for staff to learn how to use. Worse, custom-coded software has a higher risk of malfunctioning, requiring IT intervention to fix issues.
Low- or no-code technology for healthcare is ready out of the box without the need for any significant IT support. Many platforms also feature built-in tutorials that guide users through its different features and processes.
Low - or no-code technology for healthcare is ready out of the box without the need for any significant IT support.
Designed for integration
More and more technology solutions for healthcare are designed to function in several of the categories mentioned above. But for the most part, they are standalone, such as appointment scheduling platforms, or only complete specific capabilities, like invoicing and billing. These solutions need to be able to easily integrate with others to create an effective technology ecosystem.
Scaleable
An effective healthcare technology toolkit will be as easy to set up as it is to scale with evolving needs and regulations. Look for solutions with ongoing and dedicated product support by developers that continually upgrade their product. Developers of subscription or licensed no-code solutions are especially dedicated to continually update the functionality and user experience essential to a future-proof technology toolkit.
An effective healthcare technology toolkit will be as easy to set up as it is to scale with evolving needs and regulations.
Mobile-friendly
Patients now engage with their healthcare providers on mobile apps, especially for appointment intake, registration, and other patient-facing workflows. Healthcare providers often benefit from the same on-the-go-access for internal communications. Not all solutions necessarily need smartphone functionality, but it’s a useful feature to consider as you evaluate options.
How to audit your current and future technology for healthcare
Rather than starting over from scratch, audit your current tools to determine which are worth keeping. Minimizing the number of changes you make will both save time and reduce the burden on employees to learn new solutions. At the same time, evaluating your current solutions clarifies exactly what you still need. Here’s how to conduct a technology audit.
Four steps to evaluating your existing technology toolkit
- Build a stakeholder committee
- Gather feedback
- Analyze performance metrics and cost
- Research new platforms
Build a stakeholder committee
Each department has its own technology needs, so the best way to ensure these needs are met is to directly involve each one in the audit. Build a committee that consists of the leaders and technology experts in each department. This group should also include stakeholders who were involved in previous technology committees, as well as new stakeholders who may be impacted by major changes to the digital tools you use throughout your organization. Remember to include clinicians and other employees who will use the tools.
Begin by introducing each member to the implementation strategy, as well as the goals you hope to achieve. With their firsthand experience of the challenges and opportunities in their department, they may have additional insight into which goals your digital strategy should try to achieve. Each stakeholder in your committee should also identify key workers and other experts under their leadership who they can ask for additional insight.
Gather feedback
Solicit detailed overviews of all the technology each department uses, including their solutions’ capabilities, costs, and integrations. In addition to hard data, you also need to collect qualitative information to better determine how useful each tool is to employees.
Have your stakeholders conduct surveys into each technology solution in their department. They need to answer questions such as these:
- How well does this solution meet my department’s needs?
- Do employees find it easy or challenging to use?
- What important capabilities is this solution missing?
- Which solutions would employees prefer to use instead?
In addition to the fixed costs of monthly subscriptions or the flat purchase price of software, try to calculate each solution’s total cost of ownership. Consider additional parameters like its impact on labor efficiency and patient flow, or whether it generates cost savings by consolidating multiple platforms.
Analyze performance metrics and costs
Once you gather information about each tool, it’s essential to benchmark each one’s performance. In addition to the fixed costs of monthly subscriptions or the flat purchase price of software, try to calculate each solution’s total cost of ownership. Consider additional parameters like its impact on labor efficiency and patient flow, or whether it generates cost savings by consolidating multiple platforms.
Research new platforms
After clarifying exactly how each solution is performing and which needs are still unmet, you have enough information to begin your search. Outline which of your solutions you will replace, as well as the exact requirements for new tools to complete your technology toolkit. Leverage the cost and performance metrics you gathered about your current solutions to benchmark against the products you research.
As you evaluate the marketplace, always keep track of which platforms will be most compatible and easy to integrate with each other. The goal is to create a fully cohesive toolkit with as little friction as possible.

Building a better healthcare technology toolkit
Digital transformation does not end once you’ve built your healthcare technology toolkit. It’s something you need to actively maintain over time as both software capabilities and organizational needs evolve. As technology becomes more embedded in everyday processes, changes you make to your toolkit will have as much of an impact as high-level decisions about personnel and budgeting.
Follow this process to build a better toolkit.
Consolidate tools into a pillar solution
Even though digitization naturally reduces busywork and manual labor, the contextswitching it takes to use multiple solutions throughout a patient visit can cause fatigue over time. Your goal should be to upgrade user experience by consolidating individual standalone solutions into one versatile pillar solution. Limiting the number of platforms that healthcare workers engage with reduces friction throughout workflows and saves valuable mental energy.
Your goal should be to upgrade user experience by consolidating individual standalone solutions into one versatile pillar solution. Limiting the number of platforms that healthcare workers engage with reduces friction throughout workflows and saves valuable mental energy.
Examine the market to see if any end-to-end solutions can replace some of your one-off apps and software tools. Move as much as possible under a single umbrella to simplify processes, advance collaboration, reduce redundancies, and control costs.
Create a framework for iterative improvement You shouldn’t depend on vendor upgrades alone. Schedule regular reviews of your technology with your digital transformation committee to assess its current performance, changing needs, and new solutions that have entered the market. Assess the latest tech advancements and address any issues that could undermine employee retention or efficiency.
Use this opportunity to further unite your toolkit through your pillar solution. During each review, measure the impact of your last round of iterative improvements as well.
Set new performance goals
Most new technology for healthcare should have built-in monitoring to track performance metrics. Once you establish your toolkit, benchmark its current performance so you can see the value of later updates. As workflows between your various solutions become more refined, and employees get better at using the tools, it will be easy to identify areas that still need refinement.
For example, you may see a need to speed up billing cycles or reduce the average length of patient visits. Set realistic targets and examine your current processes to determine what changes to technology will help achieve it. Operational changes beyond just technology upgrades may be warranted.
Continue collecting feedback from users
Either as part of your regular review or on a revolving basis, stakeholders should continue to gather feedback from users about the current state of the technology toolkit. If multiple users complain about the convenience of a particular platform, or if the current lineup isn’t meeting certain needs, then the digital transformation committee can work together to find solutions. Implement all of this feedback during regular review cycles to avoid stretching resources too thin.
The highest priority for a digital solution is to make both providers’ and patients’ lives easier
The tools to move beyond healthcare burnout
New technology for healthcare is completely transforming the way providers care for patients. Given the extent of burnout and the impact of labor shortages, the highest priority for a digital solution is to make both providers’ and patients’ lives easier. A complete, end-toend technology toolkit is the fastest and most effective way for overburdened workers to meet the demands of the healthcare landscape with less strain on resources.
When healthcare organizations consolidate their digital resources into a comprehensive pillar solution designed especially for the needs of their industry, they invest in a platform that will become the basis for much of their future growth. As technology becomes more embedded in day-to-day operations, improving performance will become synonymous with refining your tech toolkit. With the right no-code pillar solution, your organization will have a sturdy foundation for the rest of your digital transformation now and in the future.